When To See An Allergist - Treat and Prevent Allergies | ACAAI Patient
Wheat Intolerance: The Facts
by NAOMI COLEMAN, femail.Co.Uk
An increasing number of Britons claim they are intolerant to wheat.
But far from being one condition, health problems involving wheat actually fall into three main groups.
Here is a guide to the main health conditions involving wheat in the diet, their symptoms, methods of diagnosis and treatments.
What is gluten intolerance?
Gluten intolerance - otherwise known as coeliac disease - is an inflammatory condition of the digestive tract, caused by gluten - a protein found in wheat, rye, barley and oats. It is not a contagious illness but is often genetic.
Coeliac disease affects one person in every thousand. Most people are diagnosed between the ages of 30 and 45. Classic symptoms include lethargy, weight loss, vomiting and diarrhoea.
The condition causes Gluten to damage the lining of the small intestine which greatly reduces the ability of the gut to absorb adequate nutrients from food. In the worst cases, this can lead to severe malnutrition.
Coeliac disease can be diagnosed by a gastroenterologist (stomach consultant) who will carry out an intestinal biopsy - a sample of tissue taken from the intestine.
This involves a flexible endoscope or telescope being passed through the mouth into the stomach and upper intestine so that the lining can be inspected and a biopsy taken.
The only treatment available to sufferers of Coeliac disease is a gluten-free diet.
What is a wheat allergy?
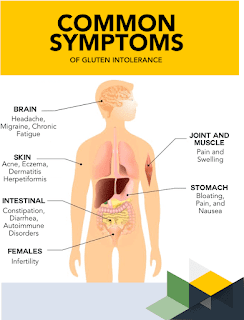
A sensitivity or allergy to wheat can produce a variety of symptoms in the body such as sneezing itching, rashes, watery eyes, runny nose, coughing, hay fever, headaches, nausea, digestive problems, swollen limbs or general aches and pains.
When someone is allergic to a certain food, their immune system reacts as if the food were an invader and produces antibodies.
Food allergies affect 1.5 per cent of the population. Wheat allergies affect less than one per cent.
Food allergies are often difficult to identify because our reactions can be delayed from anything from two hours to many days after taking the offending foods.
Common chronic illnesses and conditions such as asthma, eczema, migraines, irritable bowel syndrome and arthritis are often associated with wheat allergies.
Unlike classic allergies, if you are allergic to wheat you will usually be allergic to more than one food. On average, sufferers react to four or five different foods.
Sufferers are advised to eliminate wheat from their diet altogether and replace with rice, corn, millet, buckwheat or potatoes.
A wheat allergy can be diagnosed by skin-prick testing available at a NHS allergy clinic. This involves the allergen (wheat) being placed on the skin after it has been pricked. If the skin flares up 15 minutes later you have a wheat allergy.
A second method of diagnosis is a RAST blood test, which involves taking a blood sample and testing for the wheat allergen.
What is wheat intolerance?
Wheat intolerance does not involve an immune response. The reasons why people suffer from wheat intolerance are not entirely understood. Some experts believe it occurs when some people are short of the enzymes necessary for the proper digestion of wheat.
Symptoms of wheat intolerance can include bloating, headaches and joint pains.
However, Isabel Skypala, head of dietetics at London's Royal Brompton Hospital, believes getting a diagnosis for wheat intolerance is difficult.
'Some people find foods such as pasta and bread hard to digest. This is because pasta absorbs water, so it swells in the body and causes discomfort. Also it is fashionable to blame intolerance on wheat. People forget that other foods such as dairy which are spread on bread or sprinkled on pasta could be the offending culprit.'
The only proper diagnosis for wheat intolerance is a test called a food challenge, carried out in a hospital. The patient is blindfolded and tested for wheat under controlled conditions.
The patient is then monitored over three days to see if they develop any symptoms. Depending on which foods they react to, a food elimination programme is carried out under strict supervision.
What Should (or Shouldn't) I Eat If I Have Celiac Disease?
Celiac disease has just one clear treatment: Say goodbye to gluten. It sounds simple, but can feel overwhelming. Isn't gluten in everything?
It may feel that way at first. Because celiac affects almost 3 million Americans, gluten-free labeling is now the norm. You can find gluten-free foods on menus, grocery store shelves, and right in your own refrigerator.
That doesn't mean it's easy. Going gluten-free means rethinking how you shop, cook, and order in restaurants. With education and effort, you can make confident choices about foods that taste good and are good for you.
Gluten is a protein in wheat, barley, and rye. When those grains and the ingredients made from them (flour) are used to make foods -- like pasta, cereals, and bread -- gluten is the "glue" that holds them together.
Celiac is a genetic autoimmune disease. When you eat a food with gluten, your immune system attacks the protein. This causes damage to the villi, or little fingers that line your small intestine. Without the help of healthy villi, your body can't absorb nutrients into the bloodstream.
This causes digestive issues and malnourishment, especially when iron, calcium, and vitamin D aren't being absorbed. If it's not dealt with, celiac can cause other long-term conditions, such as neurological disorders and osteoporosis. It could also trigger the start of thyroid disease.
Support is essential. Ask your doctor to refer you to a registered dietitian who specializes in celiac. A dietitian can show you how to:
A gluten-free diet isn't as limited as you might think. In addition to prepared foods with gluten-free labels, the following foods are naturally gluten-free and the can be the foundation of healthy celiac diets:
Though you have to avoid wheat, barley, and rye, naturally gluten-free grains do exist. Use these to replace the big three:
Take a deep breath. Though the list below may contain some of your favorite foods, many have gluten-free counterparts:
Wheat, barley, and rye can appear in various forms and varieties, all of which contain gluten as well. Be sure to look out for these on food product labels:
Wheat
Rye
Barley
Triticale (a hybrid of wheat and rye)
Malt
Brewer's yeast
Wheat starch
Oats are tricky territory. Despite their nutritional benefits, and the variety they offer celiac diets, oats are often grown near wheat, barley, and rye. This opens the door to cross-contamination.
Check with your doctor or dietitian about oats labeled gluten-free.
If you have celiac disease, you might also wonder if you need to avoid casein, which is a protein in milk, butter, and cheese. If you're allergic to casein, definitely keep it out of your diet. But if you don't have a casein allergy, you might not need to worry about it.
There hasn't been a lot of research on whether casein has the same effects as gluten. The theory got its start decades ago, when some people thought that casein, gluten, and autism might be linked. That theory isn't proven.
One thing to keep in mind is that if milk upsets your stomach, it could be due to lactose, which is the natural sugar in milk. Casein and lactose aren't the same, and your sensitivity may have nothing to do with casein. Anyone can have lactose intolerance, including people who have celiac disease and people who don't.
You can ask your doctor to test and see if you're allergic to casein. If you remove casein from your diet, you'll want to focus on getting enough vitamin D and calcium.
Knowing how to read food labels is the most important part of a successful gluten-free diet. Grocery store aisles are the battleground in the fight against gluten. Take these tips with you:
When gluten-free food comes into contact with a food that has gluten, cross-contact occurs. Make sure these home hot spots are used only for gluten-free foods:
Avoiding Wheat Could Lessen Inflammation And Alleviate MS Symptoms
Multiple sclerosis (MS) is a neurological condition that affects an estimated 2.8 million people worldwide. According to the National Institute for Neurological Disorders and Stroke (NINDS), in the United States, up to 350,000 people have the disorder.
Although the exact cause of MS is unknown, scientists believe it is an autoimmune disorder, where cells that should protect a person against disease attack the body's own cells.
In MS, these immune cells break down myelin — the protective outer covering of nerve cells — and nerve cell bodies in the central nervous system (CNS). This slows down the movement of nerve impulses around the body leading to symptoms including:
Inflammation caused by the activity of immune cells can worsen MS symptoms, so taking measures to reduce inflammation may help alleviate them. That is what findings from a new study led by scientists at Johannes Gutenberg Universitat Mainz, Germany, suggest.
The study, published in Gut, found that, in mice, amylase trypsin inhibitors (ΑΤΙ), proteins found in wheat, caused inflammation in the gut, which led to inflammation in the CNS, worsening clinical symptoms of MS.
"The researchers show a diet rich in ATI can also increase CNS inflammation in mice with an MS-like condition. We don't yet know whether the same is true in people living with MS."— Dr. Clare Walton, head of research at the MS Society
Wheat, as well as other grains, contains gluten, which in some people causes a severe autoimmune reaction — celiac disease.
In people with celiac disease — around 1% of the U.S. Population — the immune system reacts when even small amounts of gluten are eaten, causing pain, bloating, and damage to the intestine, which can lead to problems absorbing nutrients from food.
Around 6% of people in the U.S. Report gluten intolerance, which also causes digestive symptoms, but these are rarely as severe as those caused by celiac disease.
However, it is not only the gluten in wheat that may cause issues. In some people, other proteins in wheat can cause inflammatory or allergic reactions, which may be serious, as Prof. Detlef Schuppan, principal investigator on the study and clinician, Medical News Today.
Prof. Schuppan, who is the director of the Institute of Translational Immunology and the Clinical Center for Celiac Disease, Intestinal Diseases and Autoimmunity, and professor of medicine/gastroenterology at the Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, noted:
"This is a long research story that goes back to one of our NIH research projects at HMS in Boston, where we discovered ATIs as activators of macrophages and dendritic cells via toll-like receptor 4 — while gluten proteins (that are responsible for celiac disease) do not have any innate immunity stimulating activity."
"This activity of the ATI proteins in wheat explained the observations that many patients have problems with wheat (so-called 'non-celiac gluten sensitivity'), which is not caused by gluten but by ATI proteins of wheat when it comes to chronic inflammatory diseases," he added.
The researchers carried out the initial investigations in mice. They used experimental autoimmune encephalomyelitis (EAE), a commonly used animal experimental model for MS.
Initially, the researchers gave female mice a gluten and ATI-free (GAF) diet for four weeks. They then divided the mice into three different diet groups:
Daily doses of both gluten and ATI were calculated to be equivalent to that consumed by a person on a standard Western diet.
The researchers induced EAE in the mice after four weeks on the GAF diet and two days before they started the experimental diets.
Those mice consuming the most ATI developed significantly more severe EAE and CNS inflammation than those consuming low ATI. Gluten alone did not have a similar inflammatory effect.
The researchers then administered ATI to monocytes — a type of white blood cell — from people with and without MS. Both released a range of pro-inflammatory chemokines and cytokines, suggesting that ATI was triggering the inflammatory responses.
In a separate pilot study, the same researchers fed a 90% wheat-reduced and a wheat-containing diet to 16 people with stable relapsing-remitting MS. They divided the participants into two groups, one started on the wheat-reduced diet, the other on the wheat-containing diet for three months, and they then crossed over for a further three months.
When on the wheat-reduced (and therefore ATI-reduced) diet, participants had fewer inflammatory immune cells in their blood and reported significantly less pain than they did when on the regular diet.
Prof. Schuppan told MNT: "If we obtain the needed funding, we will do a larger study in patients with more severe MS, where we expect an even stronger effect of the adjunctive wheat/ATI free diet."
Dr. Walton, who was not involved in the study, agreed that more research was needed.
"Based on these results, we don't know whether reducing the consumption of wheat or ATI proteins would have an effect on the symptoms of someone living with MS. […] Ideally, we need more research comparing a diet with wheat, a diet with gluten and no ATI and a diet with ATI and no gluten," she cautioned.
Dr. Walton told usthat this study alone did not provide enough evidence that people with MS should avoid wheat.
"We know people with MS are really interested in lifestyle modifications they can make to improve their MS symptoms. But so far, this new result is mostly based on animal work, so we need to see more studies in people with MS to understand how important ATI proteins are in exacerbating symptoms."— Dr. Claire Walton
However, Prof. Schuppan expressed a different opinion: "Based on our data and the positive experiences in my clinical practice, I recommend this [a wheat-free diet] to all my patients with any kind of autoimmune disease, including MS."


Comments
Post a Comment