Meat Allergy - ACAAI Public Website
What Is Severe Asthma?
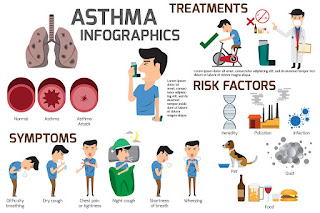
Severe asthma presents many of the same symptoms as other asthma. But it can be life threatening. You can work with your healthcare team on medications or lifestyle changes to help manage your condition.
Asthma is an inflammatory lung disease that can cause mild to severe symptoms. In most cases, avoiding triggers, taking daily medications, and using other treatment options can help you manage your asthma.
But if your asthma does not remain well managed via any type of treatment, this typically means you have severe asthma. Having severe asthma may also mean you need high doses of inhaled corticosteroids or long-term oral corticosteroids in addition to other daily medications.
Some doctors have differing opinions on the definition of severe asthma. The World Health Organization (WHO) has categorized asthma in three ways:
While severe asthma can be difficult to treat, it's still possible to manage it. Keep reading to learn the symptoms of severe asthma, signs of an attack, and treatments to manage your condition.
The symptoms of severe asthma are similar to the symptoms of mild to moderate asthma. But severe asthma symptoms tend to be more intense, potentially life threatening, and difficult to manage with asthma treatments.
Signs and symptoms of severe asthma may include:
Since severe asthma can sometimes be life threatening, make sure you know when to seek emergency medical care. If you have shortness of breath that occurs when doing simple physical activities or quickly gets worse, call 911 or go to a hospital.
If a quick-relief inhaler does not help either, you may need emergency treatment.
If you have severe asthma, your symptoms will tend to be severe, persistent, and difficult to manage, according to guidelines the Global Initiative for Asthma (GINA) developed. The WHO and National Heart, Lung, and Blood Institute created GINA in 1993.
Severe asthma either does not respond to treatments and medications at all or is very difficult to treat. This lack of response to medications is known as therapy-resistant, or treatment-resistant, asthma. It may be because your asthma has become resistant to corticosteroids or other medications used to treat asthma.
A doctor might give a diagnosis of severe asthma if you:
If your asthma is not responding to medications, talk with your doctor regarding diagnosing why it's not responding and discussing alternative treatment options.
They will check to see if you have other conditions that may be mimicking asthma, such as angina and heart failure. They will also examine you for complications of severe asthma, such as chronic infections and allergic bronchopulmonary aspergillosis.
If you have severe asthma, your doctor will work with you to develop a treatment plan. This may include medications and lifestyle changes, along with natural remedies.
Medications and treatments that a doctor may prescribe to treat severe asthma can include:
The medications listed above may be used alone or in combination to try to get your severe asthma to a manageable place.
According to research published in 2019, the following lifestyle measures may help with severe asthma symptoms:
Research indicates these lifestyle measures can be beneficial for people with asthma. However, study authors note that more research is needed regarding lifestyle interventions and asthma, as research can be inconclusive and vary depending on various factors.
While natural treatments should not replace your asthma medications, you may benefit from certain natural options in addition to your prescribed treatments.
Examples of natural, herbal remedies may include:
While research on specific herbs isn't always conclusive, there is evidence — along with centuries of practicing Chinese medicine and alternative medicine — that herbal remedies can help with lung function and benefit those with severe asthma.
Other natural treatments considered lifestyle changes may also be beneficial, including cupping, acupuncture, and massage therapy.
More research is needed on many alternative treatments and their effects on severe asthma symptoms.
It's always important to discuss any herbs or supplements you're thinking of taking with your doctor before starting them.
The symptoms of a severe asthma attack can include:
If you or your child is having symptoms of a severe asthma attack, you should call 911 for immediate medical attention. Severe asthma attacks can lead to respiratory failure, which is a life threatening condition.
The American Lung Association cites traffic light colors to indicate the three peak flow zones: green, yellow, and red. These different zones reflect how your lungs are functioning and what may be happening with your airways, to affect your asthma symptoms.
Your healthcare team may have their own guidelines or specific ranges that they follow. They can help you create an asthma action plan and address any changes in symptoms.
Severe asthma usually requires long-term treatment and medical management.
Since severe asthma can be difficult to treat, the recovery time following a severe asthma attack varies based on your individual situation and the length of time it takes to get the severe asthma attack to a manageable place.
Severe asthma can sometimes lead to lung damage, which may be permanent and may require additional treatment. That's why it's so important to get help as soon as possible during a severe asthma attack.
To help speed up your recovery, try to rest as much as you can. You may feel physically and emotionally exhausted, so take a day or more to relax and do not extend your activities beyond your healthcare team's recommendations.
Also, your doctor will likely schedule a follow-up appointment as soon as possible so they can review your symptoms and medications and adjust as needed. They can also give you recovery tips, update your asthma action plan to help prevent another attack, and answer any questions you may have.
The best way to help prevent severe asthma and severe asthma attacks is to follow the treatment plan your doctor prescribes. If your current plan is not working, let your doctor know. You can then work together to adjust it.
Here are some other ways to help you prevent severe asthma and severe asthma attacks.
Ask your doctor to help you create an asthma action plan. This action plan will outline the steps you need to take in case of an asthma attack.
It's important that you share this plan with your support network, which may include family, friends, and co-workers. By sharing your plan, they'll be able to help you if you experience an attack.
What happens if you have severe asthma?With severe asthma, usual medications will not bring relief. The symptoms will also be more extreme and last longer than they usually do with asthma. You will need to work closely with a doctor, following your treatment plan, and you may need to try several treatment combinations before finding one that works for you.
How do I know if I have severe asthma?If you have asthma that does not respond to typical asthma therapy, you may have severe asthma.
Can severe asthma go away?Severe asthma is typically a long-term condition. However, the Asthma and Allergy Foundation of America notes that around half of children with asthma "grow out of" it by the time they reach adulthood.
As their bodies develop, their airways mature and respond more effectively to airway inflammation and irritants. Their symptoms can decrease and sometimes disappear completely by the time they start school, especially if they only wheezed during viral infections and there's no family history of allergic reactions.
But some temporarily outgrow it and then experience it returning when they're older.
Can you live a normal life with severe asthma?Yes, you can live a normal life.
The treatment goal is to get your asthma to a manageable place, so it's important to consistently adhere to your doctor-prescribed treatments and lifestyle recommendations.
If you feel that your treatments are not working as they should be, discuss your concerns with your doctor. They can review treatment options.
Regularly seeing your doctor can help ensure that you continually have the best treatment plan for effectively managing your severe asthma.
If You're Living With Asthma, Here's Every Single Treatment Option Available To You
asthma-treatments-jpg
Woman using an inhaler while hiking.iStock
This summer's family barbecue was supposed to be a celebration of sorts—coming together for the first time since the pandemic pulled the plug on group activities. But your joy was cut short by an unexpected attack of coughing and wheezing. Two weeks later, a sudden tightness in your chest during a midday power walk left you gasping for air with your hands on your knees.
A trip to the doctor's office confirmed what you'd begun to suspect: You've got asthma. Like 25 million people in the U.S., you are susceptible to sudden flares of coughing and wheezing that are caused by the inflammation and narrowing of your airways, making it difficult to breathe. While developing asthma as an adult is less common than getting it as a kid, asthma rates for people of all ages are rising—one in 12 adults has asthma, according to the latest figures from the Centers for Disease Control and Prevention (CDC).
Knowing you have it is the first step; figuring out how best to treat it is the next—because right now, the condition has no cure. "Asthma is caused by a deviated immune response to your immune system," explains Dr. Corinna Bowser, MD, an allergist and immunologist with Suburban Allergy Consultants in Narberth, Pennsylvania. "We need our immune system to fight infections, therefore completely suppressing it is difficult." The good news? Treatments for the chronic condition are highly effective. The approach your doctor takes will depend on a few things, including the severity of your symptoms, the frequency of your attacks and whether certain things are more likely to trigger a flare, such as allergies or exercise.
Here's what you need to know about every asthma treatment option available to you, from over-the-counter medications to natural remedies, doctor-prescribed medications and more.
Related: An Elephant on Your Chest? Here's What an Asthma Attack Feels Like
Over-the-Counter Asthma MedicationsThere are an increasing number of products you'll find at your local drugstore claiming to solve your asthma symptoms, especially a boom in over-the-counter inhalers. Word to the wise: Don't do it. "I would not use an OTC inhaler unless cleared by your doctor," says Dr. Purvi Parikh, MD, an allergist and immunologist at NYU Langone Health in New York City. "The majority of ones that are OTC are not safe to use long term and do not treat the underlying cause. Relying on this alone without a controller and proper monitoring can lead to life-threatening asthma attacks."
Dr. Bowser agrees, adding that other OTC asthma treatments, like Primatene Mist, have side effects of increasing your heart rate while symptom relief is short-lived. "It's not a good idea in patients with heart conditions and it can also make patients shaky and anxious," she says. "Plus, if you use it several times per day, the effect gets less and less." Bottom line? "It is not a good idea to rely only on OTC asthma medications," says Dr. Bowser.
Prescription Asthma MedicationsSo what should you try? There are multiple classes of drugs that your doctor will talk with you about for treating asthma. "The one we choose depends on the severity of your asthma, which is based on pulmonary function tests, clinical history and triggers," says Dr. Parikh. Prescription asthma meds work in slightly different ways, but in general, they aim to do one of two things:
Reduce the swelling. These meds lessen the swelling and mucus in your airways. They are typically anti-inflammatories and may include steroids.
Relax the muscles. These meds loosen the grip of muscles that tighten around your airways during a flare. They are known as bronchodilators or beta-agonists.
Under that umbrella, your options are numerous. Most commonly, your doctor may prescribe inhaled medications for both short-term or long-term relief.
Inhaled corticosteroids for asthmaAsthma medication is most commonly dispensed via an inhaler (more info on inhaler options in just a minute). This is because inhaling these drugs allows them to directly interact with your airways (as opposed to going into your bloodstream) while requiring a much smaller dosage and therefore potentially fewer side effects. Inhaled corticosteroids can be taken daily or as needed. Over time, they can reduce the swelling and mucus in your airways, making it easier for air to pass through. "Inhaled corticosteroids are considered the gold standard for treatment of persistent asthma," says Dr. Bowser.
Corticosteroids are a type of anti-inflammatory drug. Your body naturally makes these steroids in your adrenal glands. But when you have asthma, your body cannot make enough to override your immune system's response, so supplementing with inhaled corticosteroids can help.
Quick-Relief Asthma MedicationsQuick-relief meds, also called rescue or short-acting drugs, are just what they sound like an 11th-hour Hail Mary when an asthma attack kicks in. "Whereas long-term and control medications treat asthma and inflammation and prevent flare-ups, quick-relief medications temporarily treat symptoms," says Dr. Parikh. "But they do nothing for the underlying condition." Quick-relief meds won't prevent further attacks, she points out, but they will ease an attack currently underway. That family barbecue might have continued as planned if you'd had a quick-relief inhaler on hand.
The most common class of quick-relief asthma medications is known as bronchodilators. These meds work by relaxing the smooth muscles that line your airways. During an asthma attack, the muscles tighten and constrict; this, combined with the swelling effect, makes it frighteningly difficult to breathe. Short-acting beta agonists (SABA) are a type of bronchodilator your doctor may prescribe, under the generic names of albuterol and levalbuterol. "Albuterol is a selective beta-agonist," says Dr. Bowser. "It will open the airways but not have as much of an effect on blood pressure and heart rate. It is intended as a stand-by medication to use as needed—it does not have a long-term effect on asthma and inflammation."
Other quick-relief drugs known as short-acting muscarinic antagonists (SAMA) may be given in conjunction with a SABA. In both cases, the drugs are typically dispensed via inhalers and last in your system for four to six hours.
Related: 10 Severe Allergy Symptoms You Should Take Very Seriously
Types of InhalersWith all this talk about inhaling your medications, you probably want to know what the deal is with asthma inhalers themselves. There are several different types, which work in unique ways to deliver medication to your airways. There is no right or wrong one to use, says Dr. Bowser: "We all are different—I have patients who love dry-powder inhalers and others hate it and get thrush from it. Some people don't like how a certain inhaler feels. It needs to be individualized for each patient." These are some of the options your doctor might talk with you about.
Metered-dose inhalerAlso known as puffers or aerosol inhalers, these devices are pre-packed with a measured amount of medication inside that is released in dose-appropriate quantities when you inhale. (You will need to prime, shake, then pump the medication into your mouth by pressing down on the canister and inhaling.) Some metered-dose inhalers include a valve-holding chamber and spacer, which help streamline the delivery of your medication. They are used for both quick relief and control medications.
Dry powder inhalerJust as it sounds, these inhalers are packed with your medication in powder form. There are no propellants or carriers as there are with aerosolized inhalers, and the powder is so fine you may not even notice that you are inhaling it. To use a dry powder inhaler, you will load the prescribed dose into the device and inhale sharply. After holding your breath for about 10 seconds, rinse your mouth out with water to prevent thrush (a fungal infection) from the powder.
Soft mist inhalerThe new kid on the block is a soft mist inhaler, which uses liquid, rather than powder or aerosolized particles. A study in the journal Clinical Drug Investigation found that soft mist inhalers deliver a greater amount of medication to the lungs and peripheral airways. It requires similar steps of priming, pumping and inhaling as metered-dose and dry powder inhalers, but because the medication is a liquid, the delivery is subtly slower and may allow for better user control, some experts believe.
Oral Asthma MedicationThough inhalers are a popular option, they rely on people following instructions and using the device exactly as intended—user error plays a large role in whether or not an inhaler treatment is successful, according to numerous studies.
Inhalers aren't the only game in town, though: Several asthma medications are available in oral pill, chewable or tablet form, as well. Corticosteroids, for instance, are available in oral form, but because they are delivered systemically via the bloodstream, the impact on your body is much greater than steroids taken with an inhaler. That can cause dangerous side effects in the long term, which is why doctors rarely prescribe oral corticosteroids for long-term asthma treatment.
Another class of oral meds is called leukotriene inhibitors. Leukotriene is a naturally occurring substance in your body that promotes inflammation; as the name sounds, these meds work to inhibit that inflammatory response. The generic drug montelukast belongs to this class of meds. "It is relatively weak in the treatment of asthma, but may help treat allergic rhinitis," says Dr. Bowser. "And it is not a steroid, so there are no steroid side effects." On the other hand, she says, the drug recently got a black box warning stating it can cause depression and nightmares.
How Biologics Treat AsthmaIf the treatments above fail to reduce the symptoms or severity of your asthma, your doctor may suggest a class of medication known as biologics. These drugs, given by injection or infusion in a medical setting, aim to block certain inflammatory molecules or antibodies in your body that trigger your immune system response. There are currently five biologics approved to treat asthma, according to the American Academy of Allergy, Asthma, and Immunology: omalizumab, mepolizumab, reslizumab, benralizumab, and dupilumab. Your treatment plan will call for a shot or infusion every two to eight weeks.
Asthma Attack Treatment PlanIf you've had asthma for a while, you start to know what might trigger an attack. Maybe it's the ragweed in September or the dust from cleaning out your garage. Whatever the trigger, if it sets off an attack, you need help, fast. What to do next depends on whether you're at home or on the road, and if you have your quick-relief (a.K.A. "rescue") inhaler with you. These steps will point you in the right direction.
How to treat an asthma attack at homeIf a large plume of dust hits you in the face as you're doing a much-needed fall cleaning of your basement, you know what's coming next. Wheezing, coughing and struggling to breathe are signs an asthma attack is unfolding. "You should immediately take two puffs of your rescue inhaler—usually albuterol," says Dr. Bowser. "If that does not work after 15 minutes, use a second two puffs and repeat every four to six hours." If the shortness of breath continues, says Dr. Bowser, contact your physician to see if another maintenance therapy can help. She cautions against repeated use of the rescue inhaler, noting that overuse of albuterol will lead to reduced response until it does not help anymore. To help yourself and others who may be around you when you're having an attack, the American Lung Association suggests filling out an Asthma Action Plan. This document will help you assess the severity of your attack and what steps to take.
Treat an asthma attack by visiting the hospitalEvery year, more than 1.6 million Americans wind up in the emergency room because of an asthma attack, according to the CDC. If your attack is so severe that you are struggling to get enough air, cannot talk, and are not responding to your rescue inhaler, head to the ER immediately. The treatment you'll get there is not necessarily so different than what you'd do for yourself at home: a dose of short-acting beta-agonists, a corticosteroid (which may be delivered intravenously in severe cases) and an additional bronchodilator to open your airways if your inhaler isn't doing the trick. The main benefit of an ER visit is simply riding out your attack in the presence of medical professionals who can employ the use of a breathing tube to help hold your airways open in life-threatening situations. Most people return home within a few hours, although in severe cases, the hospital may request that you stay overnight for observation.
What to do for an asthma attack without your inhalerAnd then, there's the case you hope never happens: You leave your house on a bike ride and multiple miles from home, you start to struggle with your breathing. You reach in your pocket for your inhaler—and discover you forgot to bring it. Your breathing gets harder, wheezing gets worse and you're on your way to a full flare without the medicine you need. Now what?
Don't panic! First step: Use your phone, or get to a phone and call for help. "You need to get to an ER," says Dr. Bowser. In the meantime, "try to breathe calmly and use your accessory muscles by leaning forward and supporting the chest by placing hands on your knees." There are other positions to take to enable accessory muscle use, she says, and these can temporarily make it easier to breathe, but it will only help in the short term.
Related: 13 Signs Your Lungs Might Not Be Healthy
How to Treat Allergy-Induced AsthmaAmong the various types of asthma (classified according to their trigger), allergy-induced asthma is the most common, affecting about 60 percent of people with the condition, according to the Asthma and Allergy Foundation of America. With allergy-induced asthma, an allergen such as dust or pollen finds its way into your body, where it triggers your immune system to release a substance called immunoglobulin E to try and rid your body of the allergen. In turn, this causes your airways to become inflamed. Although the cause of this type of asthma is specific to allergens, the symptoms (wheezing, coughing and difficulty breathing) are no different than other types of asthma, so the treatment is similar as well. Your doctor will talk with you about quick-relief and controller medications, as well as possibly allergy shots (a.K.A. Allergy immunotherapy) which introduce your body to micro amounts of the allergen to reduce your sensitivity.
Exercise-Induced Asthma TreatmentHere's a fun fact: Ninety percent of people with asthma will develop symptoms of exercise-induced asthma as well, but 10 percent of people with this condition (also referred to as exercise-induced bronchoconstriction) don't have regular asthma at all. Exercise-induced asthma occurs as you ramp up your intensity during exercise and switch from breathing through your nose to breathing through your mouth to get more oxygen. Mouth-breathing does not warm or filter the air the way nose-breathing does, and that can trigger constriction of your airways as your body tries to protect itself against the cold or dirty air. Treatment for exercise-induced asthma is similar to other forms of the condition; the main difference is that you will take your medication before exercising as a preventive measure. You can also take measures to avoid an exercise-induced asthma attack by working out indoors on days when the pollen count is high or the temperatures are very low.
Home Remedies for AsthmaGiven the challenges of living with asthma, it's natural to wonder if there's anything you can do at home to improve your situation. The answer: Yes, and no. There is very little evidence that you can treat asthma symptoms with home remedies. It's not like an itchy throat that you can soothe with a lozenge or a headache that responds to an ice pack. Asthma is a clinical medical condition that almost always requires treatment with medication. However, there are ways you can help lessen the likelihood of an attack in the first place.
HumidifierThe jury is still out on whether air-humidifying machines help or hurt people with asthma. While dry, cold air is a known trigger for some asthma patients, a study by researchers at the University of Kentucky Medical Center found that humidifying and warming the air can equally exacerbate symptoms among certain people with asthma. Moreover, "you have to be careful with humidifiers because these can grow dust mites and mold, which can make things worse," says Dr. Parikh. If you do use a humidifier, be sure to clean it frequently.
Essential oilsMost research suggests that essential oils neither benefit nor harm people with asthma, but a few small studies performed on animals suggest possible perks of essential oils for asthma relief. For instance, researchers in Japan found mice that inhaled lavender oil had lower levels of allergic inflammation and excessive mucus compared with the control group, and another study in the Journal of Experimental and Applied Animal Sciences found that exposing lab animals to eucalyptus essential oils increased the relaxation of airway muscles. On the other hand, essential oils contain what are known as biogenic volatile organic compounds, plant derivatives that can exacerbate asthma symptoms, according to recent research in the Journal of Asthma and Allergy. If you are interested in trying essential oils like lavender or eucalyptus for your symptoms, start with a small dose to see if you have adverse effects, and go from there.
Related: Essential Oils for Lungs: Are They Good or Bad?
Air purifiersIf your asthma is triggered by dust or pet dander, it makes sense that removing contact with such allergens will make it less likely you'll experience a flare. And in fact, a recent study by Korean researchers found that children with asthma who lived in homes with air purifiers used their asthma medication less than kids without the air-cleaning machines. Another study found that six weeks of using an air purifier with a HEPA filter at home significantly lowered medication use among asthmatic adults.
If you're shopping for a system to improve air quality in your home, look for a high-efficiency particulate air filter—or HEPA—which removes 99.97 percent of dust, mold and most other airborne particles in your home. But remember, air purifiers are only a good defense against asthma if your symptoms are being triggered by seasonal pollen or something else in your home. "Air purifiers with HEPA filters help if you have allergic triggers like mold or animal dander—if you don't, it won't be helpful," says Dr. Parikh.
Breathing exercises"There are some breathing exercises, like using your accessory muscles by propping your chest up on the knees or by bringing your arms over your head, which will help for a short while," says Dr. Bowser. "However when a patient has a bad asthma attack, the airways get so tight and blocked by thick mucus that breathing exercises alone will not be enough." You'll need your rescue inhaler, she says, but in the meantime, try and help your lungs by keeping your breathing calm and not hyperventilating, which will make symptoms worse.
TeaIf there's any truth to the urban lore of tea easing asthma attacks, it may come from its caffeine content. "Caffeine in large doses has a similar effect as epinephrine and albuterol," says Dr. Bowser. "However, it also has side effects just like medications—in this case, caffeine can cause the cardiac side effects of heart-racing, excited-ness and overstimulation."
Vitamins and supplementsWouldn't it be nice if you could pop a daily multivitamin and see your asthma disappear? So far, there's no evidence to suggest that's the case. But some research supports the idea that certain vitamins—C, D and E, specifically—may play a role in easing asthma symptoms. Vitamin C has anti-inflammatory properties, so it stands to reason that it could help decrease inflammation of the airways with asthma. However, the most conclusive research in Allergy, Asthma & Clinical Immunology suggests it aids primarily in cases of exercise-induced asthma, with almost no effect on other forms of the condition.
As for vitamin D, studies are inconclusive about how this vitamin may increase or decrease asthma symptoms. Because vitamin D plays an important role in the body's immune response, a lack of it may increase your risk for asthma, but researchers are still not sure. The same is true for vitamin E: Although it shares anti-inflammatory properties with vitamin C and some research shows vitamin E deficiency is linked with a higher incidence of asthma, a six-week supplementation study of asthma patients by scientists at the University of Nottingham concluded that taking vitamin E had no bearing on participants' ability to control their asthma symptoms.
Best and worst foods for asthmaJust as there are no cure-all supplements for asthma, there is no "asthma diet" either. Experts recommend a well-rounded, whole foods-based plan to reduce overall inflammation in your body. Of course, if you are allergic to, say, seafood and eating it triggers an asthma flare, you'll want to remove it from your diet. But in general, "what you eat will only affect your asthma if you are allergic to certain foods and these are your known triggers," says Dr. Parikh.
The bottom line: In small doses, natural remedies won't hurt your asthma, but they're unlikely to provide the degree of relief you're looking for. In the future, scientists may develop a cure for this condition, but in the meantime, meds are your best bet for symptom relief. "Many new monoclonal antibodies and biologic treatments are in development which seem to do a great job to reduce the disease burden of asthma," says Dr. Bowser. And that's a reason for all of us to breathe a little easier.
Up next, the surprising reasons women might get asthma as adults.
Sources:Corinna Bowser, MD, allergist and immunologist with Suburban Allergy Consultants in Narberth, Pennsylvania
Purvi Parikh, MD, allergist and immunologist at NYU Langone Health in New York City
Centers for Disease Control and Prevention: "Most recent national asthma data"
Centers for Disease Control and Prevention: "Asthma in the U.S."
Asthma and Allergy Foundation of America: "Allergens and allergic asthma."
Cleveland Clinic: "Exercise-induced asthma."
Clinical Drug Investigation: "The Respimat® Soft Mist Inhaler: Implications of Drug Delivery Characteristics for Patients."
Therapeutic Advances in Respiratory Disease: "What to consider before prescribing inhaled medications: a pragmatic approach for evaluating the current inhaler landscape."
American Lung Association: "My Asthma Action Plan."
Centers for Disease Control and Prevention: "Asthma: Healthcare Use Data 2018."
American Academy of Allergy, Asthma & Immunology: "Biologics for the Management of Severe Asthma."
American Journal of Respiratory and Critical Care Medicine: "Bronchoconstriction Triggered by Breathing Hot Humid Air in Patients with Asthma."
Life Sciences: "Lavender essential oil inhalation suppresses allergic airway inflammation and mucous cell hyperplasia in a murine model of asthma."
Journal of Experimental and Applied Animal Sciences: "Antiasthma activity of Eucalyptus grandis essential oil and its main constituent: Vasorelaxant effect on aortic smooth muscle isolated from normotensive rats."
Journal of Asthma and Allergy: "Essential oils, asthma, thunderstorms, and plant gases: a prospective study of respiratory response to ambient biogenic volatile organic compounds (BVOCs)."
Yonsei Medical Journal: "Effects of Indoor Air Purifiers on Children with Asthma."
Yonsei Medical Journal: "Effects of Air Purifiers on Patients with Allergic Rhinitis: a Multicenter, Randomized, Double-Blind, and Placebo-Controlled Study."
Allergy, Asthma & Clinical Immunology: "The effect of vitamin C on bronchoconstriction and respiratory symptoms caused by exercise: a review and statistical analysis."
Cureus: "A Review on the Role of Vitamin D in Asthma."
British Medical Journal: Thorax: "Vitamin E supplements in asthma: a parallel group randomized placebo-controlled trial."
What To Know About Coughing Up White Mucus And When To See A Doctor
Coughing up white mucus or phlegm can indicate several conditions, including asthma, bronchitis, and chronic obstructive pulmonary disease (COPD). In some cases, a person may need to see a doctor.
Mucus from the chest is responsible for protecting against microbes, and is often white or clear in color when it is healthy.
Occasionally coughing up white mucus or phlegm may not be a sign anything is wrong. However, a person may produce more mucus, or see more of it, if they have an illness that causes a cough. Doctors call this a productive or "wet" cough.
Smoke exposure is a risk factor for some of the conditions that cause this symptom. In fact, because smoke is an irritant to the lungs, avoiding secondhand smoke and quitting smoking (if applicable) may help treat a cough.
Keep reading to learn about the conditions that can cause someone to cough up white mucus or phlegm, along with the symptoms and treatments for each.
Many conditions can cause someone to cough up white mucus. Here are a few of them:
URTIsURTIs include any infection that affects the upper respiratory tract, which includes the nose, pharynx, larynx, sinuses, and large airways. Some examples of these illnesses include the common cold, influenza (flu), and COVID-19.
Viruses and bacteria cause URTIs, resulting in increased mucus production as the body tries to get rid of them. Other symptoms may include:
Depending on the illness, the symptoms may last a few days or up to 3 weeks.
If someone could have COVID-19, it is vital that they stay at home and follow the advice of their local health authority. The local health authority will have information on getting tested.
TreatmentFor viral URTIs, there is no cure. However, in most people, they are benign and get better on their own. There are over-the-counter (OTC) medications that can help reduce the symptoms while a person recovers, including:
A pharmacist or doctor can advise on the best option for an individual.
For bacterial URTIs, doctors prescribe antibiotics. Antibiotics are not appropriate for viral URTIs, but for severe cases, doctors may use antiviral medications to help the body fight the infection.
Getting the flu vaccination every year can also help prevent flu from occurring.
AsthmaAsthma is a chronic condition of the lungs that causes narrowing and inflammation of the airways. It also causes an increase in mucus or phlegm production in the air passages, which may decrease airflow while breathing. This especially affects breathing out, according to a 2021 research article.
The symptoms of asthma include:
Many things can trigger asthma symptoms, including:
TreatmentAsthma treatment may include a bronchodilator, such as albuterol (Ventolin), an inhaled steroid, such as beclomethasone (Qvar), or a combination.
Bronchitis is inflammation of the major air passages of the lungs. It causes swelling and mucus or phlegm production. Some refer to bronchitis as a "chest cold."
The potential symptoms of bronchitis include:
Common causes include:
Treatment for bronchitis depends on the cause. If it is due to a viral infection, it may get better without treatment. OTC cough medications may help relieve symptoms.
Other options include beta-agonists to reduce wheezing or steroids to reduce inflammation if the condition is ongoing.
Home remedies may include:
Lifestyle modifications also play an essential role in helping prevent recurrence. These include:
COPD is the name for a group of chronic conditions that block airflow and result in breathing problems. Symptoms include:
Exposure to tobacco smoke is a major COPD risk factor, notes the Centers for Disease Control and Prevention (CDC).
TreatmentThere is no cure for COPD. Medical treatment may involve supplemental oxygen and medications. Drug options include:
The CDC also recommends:
Mucus color can help doctors diagnose conditions. The below table shows what different colors of phlegm or mucus indicate.
Some people may wonder if the texture of the mucus or phlegm they cough up can also help with diagnosing the cause of their symptoms. However, no specific conditions are especially associated with frothy white mucus, nor solid white mucus. Mucus or phlegm can vary in consistency.
Many conditions can cause excess mucus, phlegm, or a cough. A person should contact a doctor if they:
However, if someone could have COVID-19, they should not attend a healthcare facility without calling ahead first.
If someone develops any of the following symptoms, dial 911 or the local emergency number immediately:
Mucus from the chest is often white. If a person occasionally coughs some up, it may not be a sign they have a medical condition. However, a persistent cough that produces mucus or phlegm may indicate someone has an infection, asthma, or something else.
A cough is also a common symptom of COVID-19. If someone may have COVID-19, they should seek information on getting tested.
Because this symptom can occur for many reasons, it is important to speak with a doctor about any new or unusual symptoms, particularly if they do not ease on their own.


Comments
Post a Comment