10 Eczema Types: Symptoms, Treatment and Prevention
How Your Child's Eczema Could Lead To Asthma And Food Allergies Later In Life
"It is hypothesised that an impaired skin barrier in atopic dermatitis facilitates allergen penetration, sensitisation and development of allergic diseases such as food allergy, allergic asthma and allergic rhinitis," said Dr Chong Yi Rui Tricia, a consultant with National Skin Centre.
"Scientists think this may be what leads some children to develop food allergies. When a baby's cracked skin touches food such as peanut, egg or cow's milk, their immune cells may respond and overreact to the food," said Dr Ho.
The result is the immune system's production of antibodies known as immunoglobulin E (IgE). These antibodies travel to cells that release chemicals and typically tend to create symptoms in the nose, lungs, throat or on the skin, according to American Academy of Allergy Asthma & Immunology.
Interestingly, IgE responses to inhalant allergens tend to develop later in childhood than food-specific IgE, which probably explains the delayed onset of asthma and allergic rhinitis.
Your Baby's Eczema May Be A Sign They'll Develop Asthma And Allergies In Later Life
It is common for babies to develop eczema, which appears as red, dry and itchy skin, in the first six months of their lives. (Getty Images)
The sight of red, dry and itchy skin on your baby can be worrying for new parents, but eczema is a common occurrence in infants in their first six months. According to the National Eczema Society, eczema affects around 20% of children in the UK.
But some studies have found that the presence of eczema, also known as atopic dermatitis, in babies could be linked to the development of asthma and food allergies later in life. This is known as the "atopic march".
One study, which examined children aged seven who had eczema as babies, found that 43% went on to develop asthma and 45% developed allergic rhinitis (hay fever). A separate study found that children who experienced more severe eczema as an infant had a 60% higher risk of developing asthma compared to children who had mild eczema.
Dr Sasha Dhoat, consultant dermatologist at Stratum Clinics, tells Yahoo UK that she has consistently observed the atopic march in her own clinical practice, and that about a third of babies with eczema are more likely to develop food allergies and associated respiratory disorders.
ADVERTISEMENT
Advertisement
Eczema can lead to:
A proportion of babies with atopic dermatitis may go on to develop food allergies and respiratory disorders later in life, studies have found. (Getty Images)
Atopic march: What causes it?While the progression of eczema to allergies and asthma is not linear nor predictable, Dr Dhoat explains the hypothesis that the skin condition causes "cracks" in babies' immunity.
"It is helpful to think about the epidermis, the outer layer of skin, like a brick wall to the outside world. In individuals with eczema, the brick wall, or skin barrier, is impaired, dry and cracked and it is hypothesised this allows allergen penetration, sensitization and development of other allergic diseases, over time," she says.
Dr Amer Khan of Harley Street Skin adds that genetics may also play a role in the development of conditions like food allergies, hay fever, and asthma. He points to genetic variations involves in the regulation of the immune system that have been linked to the atopic march.
"Genes associated with immune response, such as interleukins and Toll-like receptors, have been identified as potential contributors to the progression of allergic disease," he says. "Understanding these genetic factors not only provides valuable insights into the disease mechanisms but also offers exciting possibilities for personalised treatments in the future."
Eczema is thought to cause a 'crack' in the skin barrier, which therefore may expose a baby to allergens. (Getty Images)
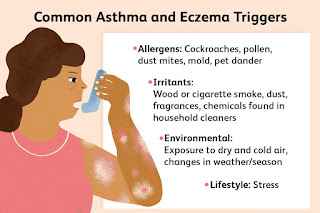
Environmental factors can also contribute to the progression from eczema to other allergies. "Allergens, pollutants, lifestyle choices, and early-life exposures can all influence the manifestation and severity of allergic diseases," Dr Khan explains, calling for a "holistic approach" to effectively manage the atopic march.
"The first step in managing this condition involves early recognition and diagnosis. Healthcare providers, including dermatologists, allergists and paediatricians, play a vital role in identifying the various components of atopic march and tailoring a treatment plan to address each individual's specific needs."
Is the atopic march preventable?Dr Dhoat says that, based on the evidence, it would appear that the maintenance and repair of the skin barrier in infants with eczema could potentially prevent the subsequent development of food allergies and asthma.
In addition, allergy testing can help identify triggers and allergens specific to individuals, which allows for targeted intervention, Dr Khan adds. "By identifying individuals at high risk based on their genetic profile, healthcare providers can intervene early, potentially reducing the burden of allergic diseases throughout their lives."
He also urges for more education and support for individuals and their families to be better able to manage the atopic march. "Raising awareness about the condition, providing guidance on skincare routines, and offering psychological support can significantly improve the overall wellbeing of those affected."
Watch: 1 in 4 people of colour with eczema feel ashamed
How do you treat eczema in babies?Dr Dhoat advises that parents begin a skin care regime that includes moisturiser, soap substitutes and topical steroids if their baby develops eczema.
Apply moisturiser regularly
Apply a moisturiser, also known as an emollient, several times a day every day to the baby's whole face and body. "The drier the skin, the more frequently moisturiser should be applied. I often recommend liberal application at every nappy change. The best moisturiser to use is the greasiest one you are prepared to apply," Dr Dhoat says.
Use a soap substitute
A soap substitute means washing with a moisturiser instead of soap. Dr Dhoat advises parents to avoid products that have a "fragrance" or "bubble" when choosing a soap substitute. "Remember infants can be internally sensitised to allergens through their cracked, dry skin, so this includes avoiding 'natural products' such as essential oils and herbal tinctures."
Apply topical steroids
Applying emollients and topical steroids in the form of ointments can help soothe and relieve eczema. (Getty Images)
Topical steroids, preferably in the form of ointments, can help relieve red, raised, cracked, and weepy areas of skin. "They come in different strengths and the doctor or specialist nurse will advise which type needs to be used, where and for how long. Use a fingertip unit to cover the same area of skin as two hands laid flat with the fingers together, or if visibly shiny, enough has been applied.
More information about skin conditions:
View comments
Dupixent: Used To Treat Eczema And Asthma
Dupixent (dupilumab) is a prescription drug that's used to treat certain inflammatory conditions, such as atopic dermatitis (a type of eczema). Dupixent comes as a solution in a prefilled syringe or prefilled pen for injection under the skin.
Dupixent is used to treat the following in certain situations:
To learn more about Dupixent's uses, see the "What is Dupixent used for?" section below.
Dupixent basicsDupixent contains the active ingredient dupilumab. (An active ingredient is what makes a drug work.) It belongs to a group of drugs called monoclonal antibodies, which are biologic medications. (A biologic is made from parts of living organisms.)
Dupilumab is available only as the brand-name drug Dupixent. It isn't available in a biosimilar form. (Biosimilars are like generic drugs. But unlike generics, which are made for nonbiologic drugs, biosimilars are made for biologic drugs.)
Doctors may prescribe Dupixent for the following conditions in certain situations:
Dupixent treats these conditions by targeting a very specific part of your immune system. Read on to learn more about these conditions and how Dupixent is used for them.
Moderate to severe atopic dermatitis (a type of eczema)Dupixent is used for atopic dermatitis in adults and children ages 6 months and older. It's prescribed when topical medications (which are applied on the skin) are not working well to control atopic dermatitis symptoms. It's also an option to try when those drugs can't be used.
With atopic dermatitis, you have dry, itchy skin patches that can flare up into rashes. Certain triggers, such as scented soaps or detergents, can cause flare-ups of this condition. Atopic dermatitis is a skin condition that's most common in children, but it can also continue into adulthood.
To treat atopic dermatitis, Dupixent can be used alone or with corticosteroids applied to the skin.
Moderate to severe asthmaDupixent is used as an add-on treatment for certain types of asthma in adults and children ages 6 years and older. (As an add-on treatment, it's used together with one or more other medications.) These types of asthma include:
Asthma is a chronic (long-term) condition that causes inflammation (swelling) and narrowing of your airways. Symptoms of asthma can include:
Certain triggers, such as exercise or cold weather, can cause asthma symptoms to suddenly become severe. This is called an asthma attack.
It's important to note that Dupixent should not be used to treat an asthma attack. Instead, you should use a rescue inhaler to ease asthma attack symptoms. Albuterol (ProAir HFA, Ventolin HFA) is an example of a rescue inhaler.
Chronic sinusitis with nasal polypsDupixent is used in adults to treat chronic (long term) sinusitis (swelling in your sinuses) with nasal polyps. (Polyps are growths on the inside lining of your nose). Dupixent is used as an add-on treatment in people who are already using other treatments, but whose symptoms still aren't well managed. (As an add-on treatment, it's used together with one or more other medications.)
Your sinuses are the hollow spaces located behind your nose, forehead, and cheekbones. Sinusitis occurs when your sinuses become inflamed (swollen) due to allergies, recurrent sinus infections, or other causes. Sinusitis symptoms usually include:
If you have sinusitis for longer than 3 months, it's considered chronic sinusitis. Over time, nasal polyps can form in inflamed sinus tissue. They can make it more difficult to breathe through your nose.
As an add-on treatment for this condition, Dupixent is used with one or more other treatments.
Prurigo nodularisDupixent is used to treat prurigo nodularis in adults.
Prurigo nodularis is a long-term inflammatory skin condition. It causes itchy, hard bumps called nodules. The itchiness can be so severe that it affects quality of life. For example, it may cause difficulties with sleep.
It's not certain what causes this condition, but it's thought to result from scratching the skin.
For treating prurigo nodularis, Dupixent is usually used alone.
Eosinophilic esophagitisDupixent is used for eosinophilic esophagitis in adults and children ages 12 years and older who weigh at least 40 kilograms (about 88 pounds).
Eosinophilic esophagitis results from an increase of eosinophils (a type of white blood cell) in the lining of your esophagus. (The esophagus is part of your digestive system. It's a muscular tube that goes from your mouth to your stomach.) This increase of eosinophils causes inflammation, and the condition is usually long term. Symptoms can vary with age and may include:
For treating eosinophilic esophagitis, Dupixent is usually used alone.
Like most drugs, Dupixent may cause mild or serious side effects. The lists below describe some of the more common side effects that Dupixent may cause. These lists don't include all possible side effects.
The common side effects of Dupixent can vary with the condition it's treating. Also, keep in mind that side effects of a drug can depend on:
Some side effects of Dupixent may continue for as long as you're receiving the drug. But no long-term side effects are known to affect people after they've stopped taking it.
If you have questions about side effects of Dupixent, talk with your doctor or pharmacist. You can also see this article for details about the drug's side effects.
Mild side effectsHere's a list of some of the mild side effects that Dupixent can cause. To learn about other mild side effects, talk with your doctor or pharmacist, or read Dupixent's prescribing information.
Mild side effects of Dupixent that have been reported include:
Mild side effects of many drugs may go away within a few days or a couple of weeks. But if they become bothersome, talk with your doctor or pharmacist. They may suggest ways to help reduce side effects.
* For more information on this side effect, see the "Side effect focus" section below.
Serious side effectsSerious side effects from Dupixent can occur, but they aren't common. If you have serious side effects from Dupixent, call your doctor right away. However, if you think you're having a medical emergency, you should call 911 or your local emergency number.
Serious side effects of Dupixent that have been reported include:
* For more information on this side effect, see the "Side effect focus" section below.
Side effect focusLearn more about some of the side effects Dupixent may cause.
Joint painJoint pain is a possible side effect of Dupixent.
Side effects of Dupixent, such as joint pain, may differ between people with different conditions. For instance, joint pain was a common side effect in studies of people who took Dupixent for chronic sinusitis (long-term sinus swelling) with nasal polyps. Nasal polyps are tissue growths inside your nose that can make it difficult to breathe through your nose.
This side effect also occurred in studies of people who took the drug for eosinophilic esophagitis. Eosinophilic esophagitis is inflammation (swelling or damage) of the esophagus. (The esophagus is part of your digestive system. It's a muscular tube that goes from your mouth to your stomach.) It's caused by a buildup of eosinophils, a type of white blood cell.
But joint pain isn't typically a common side effect in people who take Dupixent for the other conditions it's prescribed to treat.
Joints are places in your body where your bones meet, such as your elbows, hips, and knees. Joint pain may feel like an ache or soreness that can get worse when you move around.
What might help
Joint pain from Dupixent may be relieved without medical treatment.
Here are some tips that you can try at home to help ease joint pain:
If your joint pain is not relieved with these tips, or it becomes severe, contact your doctor. They might want to examine you for other causes of joint pain. Or they may suggest other ways to lessen the pain.
Eye problemsSome mild and serious eye problems have happened in people receiving Dupixent.
Conjunctivitis (pink eye) is a common side effect in people taking the drug for atopic dermatitis (a type of eczema) or prurigo nodularis (a condition that causes itchy bumps on the skin). Though less common, this side effect is also seen in people receiving Dupixent for chronic sinusitis with nasal polyps. Conjunctivitis hasn't been reported as a side effect in people taking the drug for its other uses.
Conjunctivitis symptoms may include swelling, itching, and reddening of your eye and eyelid.
Serious eye problems, such as corneal ulcers, are also possible with Dupixent. Symptoms of this condition include eye pain, blurred vision, and sensitivity to light. If you develop these symptoms, it's important to seek medical care right away.
It's also possible that Dupixent could cause eye pain or problems with your vision. If you're concerned about eye or vision problems with this medication, talk with your doctor.
What might help
Eye itching or irritation due to conjunctivitis can be bothersome, but it's usually not serious. You may find relief with just a cool compress. You could also try OTC eye itch relief drops, such as ketotifen (Alaway, Zaditor).
If you develop eye crusting or colored mucus, or a fever, you may have an eye infection. If this happens, or your eye symptoms become severe, call your doctor. They may recommend treatment with a prescription eye drop or medication.
If you notice vision changes or develop eye pain, you should not wait to see whether your symptoms get better on their own. To be safe, call your doctor. They can suggest next steps to help manage your eye problems.
Cold sores due to herpes virusDupixent does not cause infections with herpes virus. But if the virus is already inside your body, Dupixent may increase your risk of cold sores (oral herpes). Cold sores are a common side effect in people taking this drug.
Cold sores may appear on your lips or mouth. They're small, blister-like lesions that are commonly caused by the herpes virus. People sometimes notice an itch or tingling sensation in their lips or mouth before a cold sore appears.
What might help
Without treatment, cold sores usually go away on their own within 1–2 weeks.
Treatments that can help cold sores heal faster are available. Prescription medications for this purpose include penciclovir (Denavir) and valacyclovir (Valtrex). An OTC treatment such as docosanol (Abreva) may also help ease cold sores.
If you're concerned about cold sores with Dupixent, especially if you're prone to getting them, talk with your doctor. They can recommend the best treatment plan for this side effect so you'll know what to do at the first sign of a cold sore.
Allergic reaction
Some people may have an allergic reaction to Dupixent. Allergic reactions were reported in studies of Dupixent, but they were rare.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include swelling under your skin, typically in your eyelids, lips, hands, or feet. They can also include swelling of your tongue, mouth, or throat, which can cause trouble breathing.
Some people who had allergic reactions during studies of Dupixent developed the following symptoms:
Call your doctor right away if you have an allergic reaction to Dupixent. But if you think you're having a medical emergency, call 911 or your local emergency number.
Your doctor will explain how you should inject Dupixent. They'll also explain how much to inject and how often. Be sure to follow their instructions.
Injecting DupixentDupixent comes as a liquid solution in prefilled syringes or prefilled pens. Each syringe or pen contains a single dose. You'll receive Dupixent as an injection under your skin.
You can get your Dupixent injections at a healthcare professional's office. Or you may be able to get doses at home after a healthcare professional shows you or a caregiver how to administer the injection.
You can view step-by-step injection instructions for Dupixent injections on the manufacturer's website.
Dupixent injection sitesFor each Dupixent injection, you can choose one of the following injection sites:
When you choose your injection site, avoid areas of skin that are painful, bruised, or scarred. Also, it's best to choose a different site each time you inject Dupixent.
Taking Dupixent with other drugsIt's common for doctors to prescribe Dupixent along with other types of drugs.
Some examples of other kinds of drugs that you may take with Dupixent include:
If you have questions about taking other drugs with Dupixent, talk with your doctor or pharmacist.
Questions about taking DupixentHere are answers to some frequently asked questions about taking Dupixent.
Questions for your doctor
You may have questions about Dupixent and your treatment plan. It's important to discuss all your concerns with your doctor.
Here are a few tips that might help guide your discussion:
Remember, your doctor and other healthcare professionals are available to help you. And they want you to get the best care possible. So, do not be afraid to ask questions or offer feedback on your treatment.
Your doctor will recommend the dosage of Dupixent that's right for you. Below are commonly used dosages, but always take the dosage your doctor prescribes.
FormDupixent comes as a liquid solution in prefilled syringes or prefilled pens. Each syringe or pen contains a single dose. You'll receive Dupixent as an injection under your skin.
You can get your Dupixent injections at a healthcare professional's office. Or you may be able to receive doses at home after a healthcare professional shows you or a caregiver how to administer the injection.
Recommended dosageFor certain uses of Dupixent, doctors will prescribe a loading dose at the beginning of treatment. With a loading dose, a medication is started at a higher dose than the doses that follow. Loading doses get more of the drug into your body to help relieve your symptoms faster.
Dupixent's loading dose is usually given at a doctor's office. It includes two injections in two different areas of your body.
Your dosing schedule for Dupixent will be based on the condition it's being used to treat and a person's age. Below are the dosages for adults:
The pediatric dosages of Dupixent may vary for certain conditions based on a child's age, as outlined below. (Note that Dupixent is not prescribed to treat chronic sinusitis with nasal polyps or prurigo nodularis in children.)
Pediatric dosages may also vary based on weight. For more information about this and other details about Dupixent's dosage, refer to this article.
* For this use, doctors will not prescribe Dupixent to children who weigh less than 40 kilograms, or about 88 pounds.
Questions about Dupixent's dosageBelow are some common questions about Dupixent's dosage.
Costs of prescription drugs can vary depending on many factors. These factors include what your insurance plan covers and which pharmacy you use. For more information about Dupixent and cost, see this article.
If you have questions about how to pay for your prescription, talk with your doctor or pharmacist. You can also visit the Dupixent manufacturer's website to see support options.
Find answers to some commonly asked questions about Dupixent.
Is Dupixent used to treat cancer, dyshidrotic eczema, alopecia, or psoriasis?No, Dupixent is only approved to treat atopic dermatitis (a type of eczema), asthma, chronic sinusitis with nasal polyps, prurigo nodularis, and eosinophilic esophagitis. To learn about these conditions, see the "What is Dupixent used for?" section above.
But it's possible that healthcare professionals may prescribe this drug off-label for other conditions. (With off-label use, a drug is prescribed to treat a condition other than those it was approved for.)
If you have questions about Dupixent's effectiveness for other conditions, talk with your doctor.
Can Dupixent cause weight gain, hair loss, diarrhea, or headache?Dupixent should not cause weight gain, hair loss, diarrhea, or headache. These problems weren't reported as side effects during studies of the drug.
Keep in mind that other drugs may be used along with Dupixent. These drugs, such as corticosteroids, often cause multiple side effects.
If you have concerns about any side effects while you're using Dupixent, talk with your doctor.
Where can I find before and after pictures for Dupixent treatment?You can view photos of results from Dupixent treatment of adults and children with atopic dermatitis on Dupixent's manufacturer's website.
How does Dupixent work? And what's its half-life?The conditions that Dupixent is prescribed to treat are all worsened by inflammation (swelling in your body). Dupixent helps to reduce symptoms of these conditions by reducing inflammation.
Specifically, Dupixent's mechanism of action is to block certain proteins from binding to their receptors (attachment sites) in your immune system. These proteins are called interleukin-4 (IL-4) and interleukin-13 (IL-13).
Normally, when IL-4 and IL-13 bind to their receptors, your immune system releases proteins called cytokines. And this release of cytokines leads to inflammation.
The exact half-life of Dupixent isn't known. (A drug's half-life is the time it takes for your body to clear half of a dose of the drug.) But it takes about 3 months for Dupixent to be fully cleared from your system.
Is Dupixent an immunosuppressant? Does it lower the activity of your immune system?No, Dupixent is not an immunosuppressant. Instead, it's a monoclonal antibody drug, which works on very specific targets within your immune system.
Dupixent isn't known to weaken your immune system in a way that makes it easier for you to get infections. Instead, the drug reduces inflammation signals in your immune system that can cause the conditions Dupixent is used to treat, such as atopic dermatitis.
Keep in mind that inflammation signals are important for your immune system to respond to certain vaccines. For information about receiving vaccines during Dupixent treatment, see "Interactions with vaccines" in the "Does Dupixent have any interactions?" section below.
If you have questions about Dupixent's effects on your immune system, talk with your doctor.
How does Dupixent compare with Fasenra and Nucala?Dupixent, Fasenra, and Nucala are similar in that they're all monoclonal antibody drugs. (Monoclonal antibodies are large proteins that work on specific targets within your immune system.) These three medications are used for some of the same conditions, but they also have some different uses. And they contain different active drugs.
For instance, they're all used to treat eosinophilic asthma in adults and some children.
For more information on Dupixent's uses, see the "What is Dupixent used for?" section above.
Your healthcare professional can discuss the risks and benefits of the treatment options that are best for your condition.
Taking medications, vaccines, foods, and other things with a certain drug can affect how the drug works. These effects are called interactions.
Before taking Dupixent, be sure to tell your doctor about all medications you take, including prescription and over-the-counter types. Also, make a list of any vitamins, herbs, or supplements you use. Your doctor or pharmacist can tell you about any interactions these items may cause with Dupixent.
For more information about Dupixent's interactions, see this article.
Interactions with drugs or supplementsNo interactions are known to happen with Dupixent and other drugs or supplements. This is because Dupixent is a monoclonal antibody. It's broken down into pieces inside your cells.
Most other types of drugs are broken down by your liver, where they can interact with each other. Since Dupixent isn't broken down in the liver, drug interactions aren't a concern with it.
If you have questions about taking any medications or supplements with Dupixent, talk with your doctor or pharmacist.
Interactions with vaccinesDupixent reduces inflammation by blocking certain signals within your immune system. This is how the drug works to treat the conditions it's prescribed for, such as atopic dermatitis.
But these signals are important for your immune system to respond to certain vaccines. Live vaccines contain weakened versions of viruses or bacteria.
So, you should not get live vaccines while you're receiving Dupixent. If your immune system doesn't respond the way it should, you could get the infection a live vaccine is meant to protect you from.
Talk with your doctor to make sure that your vaccines are up to date before starting Dupixent treatment. If you need any live vaccines, they'll likely have you wait to start Dupixent until at least 4 weeks after you get any live vaccines.
Examples of live vaccines include:
Non-live vaccines are generally safe to get while you're receiving Dupixent. Some common non-live vaccines include:
If you have questions about getting vaccines while taking Dupixent, talk with your doctor or pharmacist.
Before you take Dupixent, talk with your doctor about your overall health and any medical conditions you may have. Your doctor can recommend whether this drug is safe for you. Factors to consider include those described below.
Taking or stopping steroid medicationsIf you're taking Dupixent, your doctor will likely prescribe additional medications for your condition, such as corticosteroids. Examples include oral prednisone, inhaled fluticasone (Flovent) or budesonide (Pulmicort), and nasal fluticasone (Flonase).
You should not suddenly stop taking steroid drugs. Doing so may cause side effects such as nausea, vomiting, or fatigue (low energy). If your doctor recommends you stop taking a steroid, talk with them about how to slowly lower your dosage before completely stopping the drug.
Also, if you have asthma and take a steroid by mouth, Dupixent may increase your risk of problems related to eosinophilia. (With eosinophilia, you have an increased level of eosinophils, which are a type of white blood cell that cause swelling.) In rare cases, severe vasculitis (swelling throughout your blood vessels) has occurred with eosinophilia.
If you take steroids for asthma, talk with your doctor before starting Dupixent. They may monitor you more closely while you're receiving this drug.
Eye or vision problemsDupixent can cause new or worsening symptoms of eye or vision problems. It's important to have frequent eye exams while taking Dupixent. Be sure to talk with your doctor if you develop any eye symptoms or vision changes while taking this drug.
Parasitic infectionsIf you have a parasite (worm) infection, such as tapeworm or roundworm, you'll need treatment for it before you start using Dupixent. If you get a worm infection during Dupixent treatment, your doctor may recommend you stop taking the drug until the infection has been treated.
This is because Dupixent wasn't studied in people with worm infections. So, it isn't known whether Dupixent may lower your immune system's ability to clear this type of infection.
Joint painJoint pain can be a side effect of Dupixent. The drug can also make any existing joint pain worse. If you have a history of joint pain or you experience new or worsening joint pain while taking Dupixent, tell your doctor. They might recommend seeing a specialist or stopping Dupixent treatment if your symptoms don't get better.
VaccinesMake sure all your vaccines are up to date before you start Dupixent treatment. Your doctor can help make sure you have all the vaccines you need for your age. This is important because some vaccines aren't safe to receive with Dupixent. See "Interactions with vaccines" in the "Does Dupixent have any interactions?" section just above for details.
Asthma attacksWith asthma, symptoms such as shortness of breath and wheezing can become suddenly severe. This is called an asthma attack. Dupixent should not be used to stop an asthma attack. Instead, a rescue inhaler, such as albuterol (ProAir HFA, Ventolin HFA), should be used.
Allergic reactionIf you've had an allergic reaction to Dupixent or any of its ingredients, you should not take Dupixent. Ask your doctor about other treatment options that would be safer for you.
Alcohol may cause harmful interactions when taken with certain drugs, but Dupixent isn't one of them.
If you drink alcohol and you're wondering how much is safe to drink with your condition, talk with your doctor.
It isn't known if Dupixent is safe to take during pregnancy or while breastfeeding. If you're pregnant, breastfeeding, or planning either, talk with your doctor. They can recommend the safest way to treat your condition during this time.
If you use Dupixent while pregnant, you might consider joining the drug's pregnancy registry. A pregnancy registry monitors the health of people who take a certain drug during pregnancy. You can call 877-311-8972 or visit the registry's website for more information or to sign up. You can also talk with your doctor.
Dupixent (dupilumab) and Xolair (omalizumab) are both biologic drugs. They're made from living cells rather than chemicals. Both drugs are types of monoclonal antibodies. They work by targeting very specific but different parts of your immune system.
Dupixent works by blocking inflammation signals. Xolair works by blocking a protein that's involved in allergic reactions.
Dupixent and Xolair are both used to treat certain forms of asthma in adults and some children. They each have other uses, too.
You can learn more about how they are alike and different in this article. Also, be sure to talk with your doctor about which drug is better for you.
In some cases, your doctor may recommend that you take a drug other than Dupixent, depending on the condition you have.
Some of the drugs listed below are used off label for these conditions. With off-label use, a drug that's approved for certain conditions is used for another condition.
Alternatives for atopic dermatitis (eczema)Other treatments for atopic dermatitis (a type of eczema) include:
Other drugs for asthma include:
* See the "What should I know about Dupixent vs. Xolair?" section just above for more information.† See "How does Dupixent compare with Fasenra and Nucala?" in the "What are some frequently asked questions about Dupixent?" section above for more information.
Alternatives for chronic sinusitis with nasal polypsOther treatments for chronic sinusitis with nasal polyps include:
* Budesonide is typically inhaled. But for this use, which is off-label, the drug is swallowed.
Do not use more Dupixent than your doctor prescribes. Taking more than this may lead to serious side effects.
What to do in case you take too much DupixentCall your doctor if you think you've used too much Dupixent. You can also call 800-222-1222 to reach America's Poison Centers, or use its online resource. However, if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
If you have certain forms of atopic dermatitis, asthma, chronic sinusitis with nasal polyps, prurigo nodularis, or eosinophilic esophagitis, your doctor may prescribe Dupixent for you.
When you're considering using Dupixent, it's important to talk with your doctor about your treatment plan. It's common to continue using other treatments for atopic dermatitis, asthma, or chronic sinusitis with nasal polyps during Dupixent treatment. Be sure that you understand which treatments you should continue using. And ask your doctor if there are any you should stop using.
You may also want to discuss other ways to manage your symptoms besides using medication. For example, with atopic dermatitis, these may include avoiding certain triggers and trying natural remedies.
Here are some other questions to ask when talking with your doctor:
To learn more about Dupixent, see these articles:
To get information on different conditions and tips for improving your health, subscribe to any of Healthline's newsletters. You may also want to check out the online communities at Bezzy. It's a place where people with certain conditions can find support and connect with others.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.


Comments
Post a Comment